Emergence of a Deadly Coronavirus
Aerosol Transmission
Singing indoors, unmasked can swiftly spread COVID-19 via microscopic airborne particles known as aerosols, confirms a new peer-reviewed study of a March choir rehearsal which became one of the nation's first superspreading events.
"This study documents in great detail that the only plausible explanation for this superspreading event was transmission by aerosols. Shared air is important because you can be inhaling what someone else exhaled even if they are far away from you," said Shelly Miller, lead author on the study and professor of mechanical engineering.
On March 10 in Skagit Valley, Washington, one person with mild symptoms of COVID-19 attended a 2.5-hour choir practice indoors. In the weeks that followed, more than 50 other people from that rehearsal would contract the disease—almost everyone who attended—and two died. Because participants had taken precautions to sanitize and avoid touching each other, scientists suspected that aerosol transmission, not larger drops spit into the air or infected surfaces, were the culprit.
The new paper, published this week in the journal Indoor Air, confirms it.
Members of the chorale were serious about their music and their health that day. They did not touch each other, touched few shared surfaces, propped doors open and used hand sanitizer. Few people shared the same restroom as the infected person, and many who did not use any restroom got sick.
They did not, however, wear masks.
By interviewing the chorale through a representative about what happened that day and calculating the rate of infection based on the details of the rehearsal and what is known about the SARS-CoV-2 virus, researchers conclude that there simply were not enough opportunities for droplets and infected surfaces, known as fomites, to transmit the virus to the number of people who fell ill afterwards.
But poor ventilation in the indoor space led to a build-up of aerosols produced by the singers, and heat produced by the singers themselves mixed the air within the room.
There were also many singers present and the rehearsal was long.
"The inhalation of infectious respiratory aerosol from 'shared air' was the leading mode of transmission," said Jose-Luis Jimenez, co-author of the study, professor of chemistry and fellow at the Cooperative Institute for Research in Environmental Sciences (CIRES).
The researchers found that shortening the rehearsal time in the Skagit Valley event from 2.5 hours to 30 minutes would have dropped the rate of infection from 87% to 12%. Wearing masks, improving ventilation, using portable air cleaners and rehearsing for half of the duration combined could have dropped the number of people infected down from 52 to only 5, in a subsequent analysis using a widely-available tool developed by Jimenez, Miller and colleagues based on the study.
This superspreading event happened early on in the pandemic, when there were no known cases in Skagit County. Businesses were just starting to shut down in the U.S. and public health officials were just beginning to debate whether masks were necessary. Aerosols, floating pieces of bodily fluids much, much smaller than droplets that also can carry the novel coronavirus, could not be responsible for COVID-19, said the World Health Organization (WHO) and Centers for Disease Control (CDC). Wash your hands and stand six feet apart, they said.
But after hearing of the outbreak in Washington state, Miller wasn't convinced.
"Singing is known to release high amounts of aerosol," Miller said.
Since March, other choir superspreading events have also occurred in the Netherlands, Austria, Canada, Germany, England, South Korea, Spain and France.
The new study offers new insight into how those outbreaks occurred and what can be done to make future choral rehearsals safer.
The authors recommend conducting choral practices outdoors whenever possible during the COVID-19 pandemic, and carefully managing any indoor singing events, as singing can generate large amounts of aerosolized virus if any of the singers is infected. Improved ventilation which draws in more outside air, and air cleaning, that removes virus-containing aerosols from the air, can be helpful to reducing the spread of airborne infections in any indoor space, but singing with masks and at distances more than 6 feet apart are very important as well.
Miller and her fellow researchers first submitted their results in June, but aerosols are still not being openly acknowledged by the WHO and CDC as an important route of transmission for SARS-CoV-2.
"The research adds to the overwhelming body of evidence that aerosol transmission is playing a major role in driving this pandemic and especially to superspreading events," said Jimenez.
Source: Singing unmasked, indoors spreads COVID-19 through aerosols, new study confirms
_________________
Author of Practical Preparations for a Coronavirus Pandemic.
A very unique plan. As Dr. Paul Thompson wrote, "This is the very best paper on the virus I have ever seen."
World Health Organization - I Respectively Disagree
This article is a few months old and I may have cited it before, but it is worth repeating.
For months, the World Health Organization (WHO) has said COVID-19 spreads mainly via direct contact with large respiratory droplets, like those expelled in a sick person’s cough or sneeze. In a letter published this week in Clinical Infectious Diseases, 239 scientists say the agency may be wrong.
It’s only the latest chapter in an ongoing tug of war between the WHO and the rest of the public-health world. “This is one in a series of many miscues,” says Dr. Eric Topol, director and founder of the Scripps Research Translational Institute. “It’s really unfortunate how the WHO has led to all sorts of confusion.”
The new letter, which was co-written by a WHO consultant and reviewed by experts from more than 30 countries, argues the WHO and other health authorities are not paying enough attention to airborne COVID-19 transmission—that is, infection via inhaling tiny respiratory droplets that can linger in the air.
WHO officials acknowledged that possible route of transmission at a press conference Tuesday, after the letter was published, but said it continues to collect evidence. “We have been talking about the possibility of airborne transmission and aerosol transmission as one of the modes of transmission of COVID-19,” Maria Van Kerkhove, the WHO’s technical lead for COVID-19, said.
Studies of other viruses completed before the pandemic have “demonstrated beyond any reasonable doubt” that droplets expelled by sick individuals can “remain aloft in air and pose a risk of exposure at distances beyond 1 to 2 [meters] from an infected individual,” the letter says. More recent research suggests the same is true of SARS-CoV-2, the virus that causes COVID-19. In some reported cases, people have gotten sick after being in the same room as an infected individual, even if they didn’t have close or sustained contact.
Think of it like cigarette smoke, says Linsey Marr, a professor of civil and environmental engineering at Virginia Tech and one of the letter’s signatories. The cloud is most concentrated around the person smoking, but it also disperses and drifts throughout the room. Viral aerosol functions much the same way, she says.
The WHO’s COVID-19 guidance has addressed airborne spread in health care environments, since some procedures can aerosolize the virus, but stopped short of calling it a threat to the general public. A WHO spokesperson told TIME “the topic is presently being reviewed by our technical experts.”
The letter’s 239 signatories say that’s not good enough. “There’s been a lot of emphasis on hand-washing and on social distancing, but if they [the WHO] acknowledge that aerosol transmission is happening, we can have additional guidance” about things like ventilation techniques and wearing masks whenever people congregate indoors, Marr says. Even very simple guidance, like keeping doors and windows open when possible, could help, she adds.
There’s nothing to stop cities or countries from codifying these sorts of precautions on their own. But as the world’s preeminent global health authority, the WHO’s words—and silence—carry weight. If the WHO doesn’t publicly recognize risks like airborne transmission, “it just gives naysayers more fodder to deny the truth,” Topol says.
The letter is only the latest example of the roiling tension between the WHO and the wider scientific community.
The fast-moving COVID-19 pandemic has exposed the WHO’s weak spots. For one thing, the underfunded and overburdened global health agency cannot enter countries to do fieldwork without permission, and relies on its member states to provide much of the data used in its analyses.
The WHO also moves with the slow pace and risk aversion of a bureaucratic organization, even when the world is demanding new and better information about the coronavirus every day. “The evidence for aerosol transmission is there; it’s just maybe not as compelling as they would like,” Topol says. “I call it a purist view.”
That institutional caution helps explain why it took the WHO until June 5 to recommend that people in high-transmission areas wear fabric face masks in public—a recommendation that was, by then, already standard in many countries and cities. “Every recommendation that we put out needs to be applicable for every type of situation. That’s a blessing and a curse,” Van Kerkhove told TIME when the mask guidance came out.
Topol says that bar is sometimes too high. “What do you have to lose” by recommending extra precautions, he asks. “Go with the best evidence and the best expert opinion. Maybe it’s not perfect evidence. But it’s good enough.”
Despite holding press briefings almost every day, the WHO has also stumbled when communicating with the general public. In an oft-criticized tweet from January, for example, the WHO declared that, “Preliminary investigations conducted by the Chinese authorities have found no clear evidence of human-to-human transmission of the novel #coronavirus.”
To the WHO, that mean the threat of widespread human-to-human transmission—though possible—was still under investigation. To the average person, it meant human-to-human transmission wasn’t a big threat. So when it became clear that COVID-19 does pass from person to person, many people lost faith in the WHO.
For many, that feeling was compounded last month when Van Kerkhove called asymptomatic coronavirus transmission “very rare” during a press conference, despite several studies and months of expert warnings to the contrary. She later walked back the comment.
These incidents are more than communication slip-ups. Topol fears they’ll erode trust in the WHO—and in science more broadly—at the exact moment that confidence is critically important.
“WHO is a venerable institution, something that we need, that we rely on,” Topol says. “Each time one of these things happens, where there’s a serious misalignment with the truth and the science and the evidence, you wind up with another credibility titer reduction. We need to go the other direction.”
Source: The WHO Says Airborne Coronavirus Transmission Isn't a Big Risk. Scientists Are Pushing Back
_________________
Author of Practical Preparations for a Coronavirus Pandemic.
A very unique plan. As Dr. Paul Thompson wrote, "This is the very best paper on the virus I have ever seen."
COVID Transmission Among Young People
The Centers for Disease Control and Prevention just updated its COVID-19 statistics on kids. This is what they found.
For persons under 21 years of age during the period February 12 - July 31, 2020.
* There were a total of 391,814 cases of COVID-19
* Multi-inflammatory syndrome in children (MIS-C) was reported in 8% of these cases
* There was 121 death. This represented 0.03% of all cases among children and 0.08% among all reported deaths.
“…although Hispanic, Black, and AI/AN persons represent 41% of the U.S. population aged <21 years (4), these groups accounted for approximately 75% of deaths in persons aged <21 years. …deaths were more prevalent among males
* …among persons aged 10–20 years, [with] young adults aged 18–20 years accounted for nearly half of all deaths in this population.
* 75% of decedents had at least one underlying condition, and 45% had two or more underlying conditions.” These conditions included asthma 28%, obesity 27%, neurologic or developmental conditions 22% and cardiovascular disease 22%.
* For perspective, in the absence of an underlying condition, the chance of dying was 0.0075%
* Almost a third of the deaths occurred at home or in the Emergency Department (ED). This suggests that the disease was under-recognized, under managed, or very aggressive in its time course. This is consistent with a decline in ED services during this period.
This data shows that nearly three quarters of SARS-CoV-2–associated deaths among infants, children, adolescents, and young adults have occurred in persons aged 10–20 years, with a disproportionate percentage among young adults aged 18–20 years and among Hispanics, Blacks, AI/ANs, and persons with underlying medical conditions
Source:
CDC Reports Latest Aggregate Data On COVID-19 And Children
SARS-CoV-2–Associated Deaths Among Persons Aged <21 Years — United States, February 12–July 31, 2020
_________________
Author of Practical Preparations for a Coronavirus Pandemic.
A very unique plan. As Dr. Paul Thompson wrote, "This is the very best paper on the virus I have ever seen."
Change in CDC Protocol
The Centers for Disease Control and Prevention reversed course again Friday, now recommending that people get tested if they come into contact with someone who has coronavirus, even if they are asymptomatic.
"Due to the significance of asymptomatic and pre-symptomatic transmission, this guidance further reinforces the need to test asymptomatic persons, including close contacts of a person with documented SARS-CoV-2 infection," the CDC's updated guidance says.
Close contact means coming "within 6 feet of a person with documented SARS-CoV-2 infection for at least 15 minutes." The CDC also recommends that even if you test negative, you should still self-isolate for two weeks because a "single negative test does not mean you will remain negative at any time point after that test."
Source: CDC reverses course again, says asymptomatic people should be tested
_________________
Author of Practical Preparations for a Coronavirus Pandemic.
A very unique plan. As Dr. Paul Thompson wrote, "This is the very best paper on the virus I have ever seen."
Apple Watch Series 6 and the Coronavirus
I read a review of the new Apple Watch called Series 6. It has one interesting feature that is related to the coronavirus.
It will let people measure their blood oxygen levels right from their wrists. Why is this important? Because one of the early signs of contracting the coronavirus is a drop in blood oxygen levels. Earlier in this thread, I recommended people buy an oximeter to monitor their blood oxygen levels.
In fact, there's a phenomenon we've observed clinically where a person with COVID-19 can have very low oxygen levels but otherwise appear well, termed "happy hypoxia." It's concerning because these patients may be more significantly ill than they feel, certainly warranting closer attention in a medical setting.
It's why you may be wondering if an oximeter can help detect COVID-19 early.
Source: Can an Oximeter Help Detect COVID-19 at Home?

The new watch, which went on sale on Sept. 18, also comes with an S6 dual-core processor that is optimized for Series 6 and a new chip that will make the watch about 20% faster than the Series 5. It also comes with an optimized display that makes it easier to view in bright sunlight.
"Most of the new features that I can’t speak to yet are ones that require a couple of days to test out -- sleep tracking, long-term VO2 max calculations and blood oxygen measurements being the most important among them," Palladino penned.
Source: Apple Watch Series 6 review roundup: Should you buy one?
So if you want continuous monitoring of your blood oxygen levels and an early heads up if your lung function is being degraded by COVID-19, this may be the watch for you.
I also noticed this watch measures VO2 Max. VO2 max refers to the maximum amount of oxygen you can utilize during exercise. Why might this be important? Well Aspies suffer from a high degree of stress. This stress energy (a cascade of hormones) is stored in our muscles and nervous system. Our bodies are not really designed to store this stress for long periods of time and eventually the stress will transition into distress (such as depression, anxiety, panic attacks and a host of mental illnesses.) This stress energy can be vented from the body but it takes a certain type of extreme exercise to make this happen. So light and moderate exercise normally only reduces stress levels for a few minutes. For the stress reduction effects of exercise to be long lasting, one needs to perform maximal or supramaximal exercise. This is exercise where the intensity or individual’s maximal oxygen uptake (percentage of VO2max) is 100% or greater. Examples are sprints and power exercises. So the watch becomes an instrument to measure VO2 Max which can be used as a measure of venting stress energy in the arms and legs.
I guess when the battery dies on my current Fitbit, I may have to buy one of these. Especially since one of my special interest is "the latest gadgets."
_________________
Author of Practical Preparations for a Coronavirus Pandemic.
A very unique plan. As Dr. Paul Thompson wrote, "This is the very best paper on the virus I have ever seen."
The CDC has FINALLY updated its Guidelines to incorporate Aerosol transmissions.
COVID-19 most commonly spreads
* Between people who are in close contact with one another (within about 6 feet).
* Through respiratory droplets or small particles, such as those in aerosols, produced when an infected person coughs, sneezes, sings, talks, or breathes.
-------These particles can be inhaled into the nose, mouth, airways, and lungs and cause infection. This is thought to be the main way the virus spreads.
--------Droplets can also land on surfaces and objects and be transferred by touch. A person may get COVID-19 by touching the surface or object that has the virus on it and then touching their own mouth, nose, or eyes. Spread from touching surfaces is not thought to be the main way the virus spreads.
* It is possible that COVID-19 may spread through the droplets and airborne particles that are formed when a person who has COVID-19 coughs, sneezes, sings, talks, or breathes. There is growing evidence that droplets and airborne particles can remain suspended in the air and be breathed in by others, and travel distances beyond 6 feet (for example, during choir practice, in restaurants, or in fitness classes). In general, indoor environments without good ventilation increase this risk.
Source: Coronavirus Disease 2019 (COVID-19)
So what does that mean? Well it means that if you want to protect yourself from COVID-19 you need to wear a mask when you are in areas where there is a large viral load, such as indoors, in mass transit, in poor ventilated areas. But not just any mask, but rather one that can filter out these microscopically small viral particle, and that mask is an N95. This will go a long ways especially in the dry winter months ahead in keeping you safe from infection.
_________________
Author of Practical Preparations for a Coronavirus Pandemic.
A very unique plan. As Dr. Paul Thompson wrote, "This is the very best paper on the virus I have ever seen."
The CDC just did a Double Take!
CDC deletes coronavirus airborne transmission guidance, says update was 'draft version'
The Centers for Disease Control and Prevention issued a correction on its website Monday, saying a draft of proposed changes, including guidance on airborne transmission of coronavirus, was posted in error.
“A draft version of proposed changes to these recommendations was posted in error [on Friday] to the agency’s official website. CDC is currently updating its recommendations regarding airborne transmission of SARS-CoV-2 (the virus that causes COVID-19). Once this process has been completed, the updated language will be posted,” as written on the website.
All of the previously published language in the "draft version" on Friday regarding airborne transmission was removed from the webpage before noon on Monday.
--------------------------------------------
TOO BAD, SO SAD - BUREAUCRACY THAT MOVES AT LETHARGIC SNAIL SPEED IN HIGH GEAR!
_________________
Author of Practical Preparations for a Coronavirus Pandemic.
A very unique plan. As Dr. Paul Thompson wrote, "This is the very best paper on the virus I have ever seen."
Airborne vs. Aerosol vs. Droplet: What's the Difference?
COVID-19 has introduced several new terms to the national lexicon. In addition to phrases like social distancing, self-quarantine, and N95 respirator, you may have seen the word airborne popping up more in recent weeks. It usually appears in discussions concerning how the novel coronavirus that causes COVID-19 is transmitted—a question that's still debated by health experts. So what exactly does it mean when a pathogen is airborne, what do droplets and aerosol have to do with it, and which of these terms apply to the new coronavirus?
We know that there are at least two ways to catch the new coronavirus: by coming in close contact with infected individuals and touching contaminated objects and surfaces. In both cases, the root of the transmission is often a cough or sneeze. When someone with COVID-19 coughs—which is a common symptom of the disease—they send a spray of mucus and saliva droplets flying from their mouths. These tiny, sometimes invisible droplets, measuring between five and 10 micrometers in diameter, contain particles of the virus. Coughing into a shirt sleeve or mask can catch a lot of these droplets, but with nothing to block them, many will land on objects and people in the immediate vicinity. This is why a sick person is more likely to infect more people standing elbow-to-elbow with them in crowded subway car than they are keeping a 6-foot distance from others in a spacious park.
You don't need to be touching someone to contract coronavirus from them. If someone is standing directly behind you in line at the grocery store, they can infect you through the droplets in a sneeze or cough. But while these droplets technically travel through the air, that doesn't automatically make COVID-19 an airborne disease—at least not according to the definition of the word used by health officials. In order to understand what airborne really means, you need to know about aerosols.
What are aerosols?
Saliva and mucous droplets are heavier than air, which means gravity starts pulling them—and whatever viral particles they contain—towards the ground as soon as they leave someone’s body. By the time someone walks out of a room, any droplets they may have emitted have likely already settled on the floor or nearby surfaces—so usually, you don’t need to worry about breathing in those droplets if you’re social distancing correctly.
Aerosols are a different story. They form when smaller droplets evaporate faster than they fall to the ground, leaving nuclei measuring less than five micrometers in diameter. Without heavy liquids dragging them down, virus particles from these evaporated droplets are able to float through the air for up to half an hour. When a virus travels via aerosols, it’s possible to contract it by entering an empty room that a sick person was in several minutes earlier. This transmission via free-drifting aerosols is how the World Health Organization defines an airborne disease.
Is the new coronavirus airborne?
The WHO updated its scientific brief in July to say that airborne transmission of the new coronavirus appears to be possible. Citing three studies of infections in a gym, a choir practice, and a restaurant, WHO stated, "short-range aerosol transmission, particularly in specific indoor locations, such as crowded and inadequately ventilated spaces over a prolonged period of time with infected persons, cannot be ruled out."
Though there may be a chance of the novel coronavirus wafting in ambient air, it's not unsafe to open a window or go outside. Airborne viruses are more likely to spread in rooms with poor ventilation than they are outdoors, so allowing air to circulate in your home can actually help prevent the spread of disease. Plus, getting fresh air and exercise is important for staying mentally and physically well in stressful situations.
When leaving the house, just keep some safety precautions in mind. Maintain at least a 6-foot distance from others to protect yourself from droplet transmission, and wash your hands thoroughly after touching surfaces that may be contaminated. Wearing an N95 respirator is the best way to prevent airborne infection, but because supplies are limited, new masks should be reserved for especially vulnerable people like healthcare workers. Homemade cloth masks and surgical masks aren’t built to filter out smaller airborne particles, but they can stop larger droplets from splashing onto your face, and just as importantly, stop infected wearers from spreading droplets to others.
Source: Airborne vs. Aerosol vs. Droplet: What's the Difference?
_________________
Author of Practical Preparations for a Coronavirus Pandemic.
A very unique plan. As Dr. Paul Thompson wrote, "This is the very best paper on the virus I have ever seen."
ASPartOfMe
Veteran

Joined: 25 Aug 2013
Age: 66
Gender: Male
Posts: 34,465
Location: Long Island, New York
Coronavirus spike pushes Canadian authorities to step up powers to limit large gatherings
Officials in the province of Quebec and in the country's capital, Ottawa, have declared that a second wave has already taken hold in their cities and communities. Canada's seven-day average is now just under 1,000 cases per day, according to Johns Hopkins University and the Public Health Agency of Canada.
"I'm telling you that right now the curve is not the way it was in the Spring, but it's still pretty bad," said Dr. Horacio Arruda, Quebec director of public health during a press conference in Quebec City Monday. "If we don't do something it's going to go up even more, and I'm telling you that will not be fun."
Across the country, public health experts say Canadians are having too many close, social contacts between family and friends and young people are gathering in groups that are too large to contain the spread. Canadian government statistics show that about two thirds of new, positive cases of coronavirus are detected in people under the age of 40.
_________________
Professionally Identified and joined WP August 26, 2013
DSM 5: Autism Spectrum Disorder, DSM IV: Aspergers Moderate Severity
It is Autism Acceptance Month
“My autism is not a superpower. It also isn’t some kind of god-forsaken, endless fountain of suffering inflicted on my family. It’s just part of who I am as a person”. - Sara Luterman
Andoras
Yellow-bellied Woodpecker

Joined: 19 Nov 2014
Age: 35
Gender: Male
Posts: 61
Location: Dunakeszi, Hungary
Finally, I found the English version:
https://semmelweis.hu/english/2020/09/t ... -believed/
Researchers of Semmelweis University were able to study the structure of the active and infectious coronavirus in collaboration with the researchers of the National Security Laboratory of the National Centre for Public Health. Based on their results, the corona-shaped spikes covering the surface of the virus are extremely flexible, the virus has the ability to self-heal and may be one of the most resilient biological organisms known to humanity. Their study proves that the coronavirus can easily be compressed but restores its shape like a rubber ball and its structure is not damaged by physical impact. All these could greatly contribute to its unusually high infectivity.
What do you think?
According to Johns Hopkins University researchers, out of 20 nations worldwide they track, the U.S. is ranked 11th in COVID-19 case mortality rate. Mexico accounting for the highest rate at 10.5 percent. By comparison, the U.S. has a 2.9% rate, falling behind other countries including France, Spain, Romania, Colombia and Brazil.
The observed case-fatality ratio figures measure the number of deaths per 100 confirmed cases. The researchers noted that countries with more testing and more instances of mild cases may have a lower case-fatality ratio than others, and that factors such as older populations and health care systems may impact the results.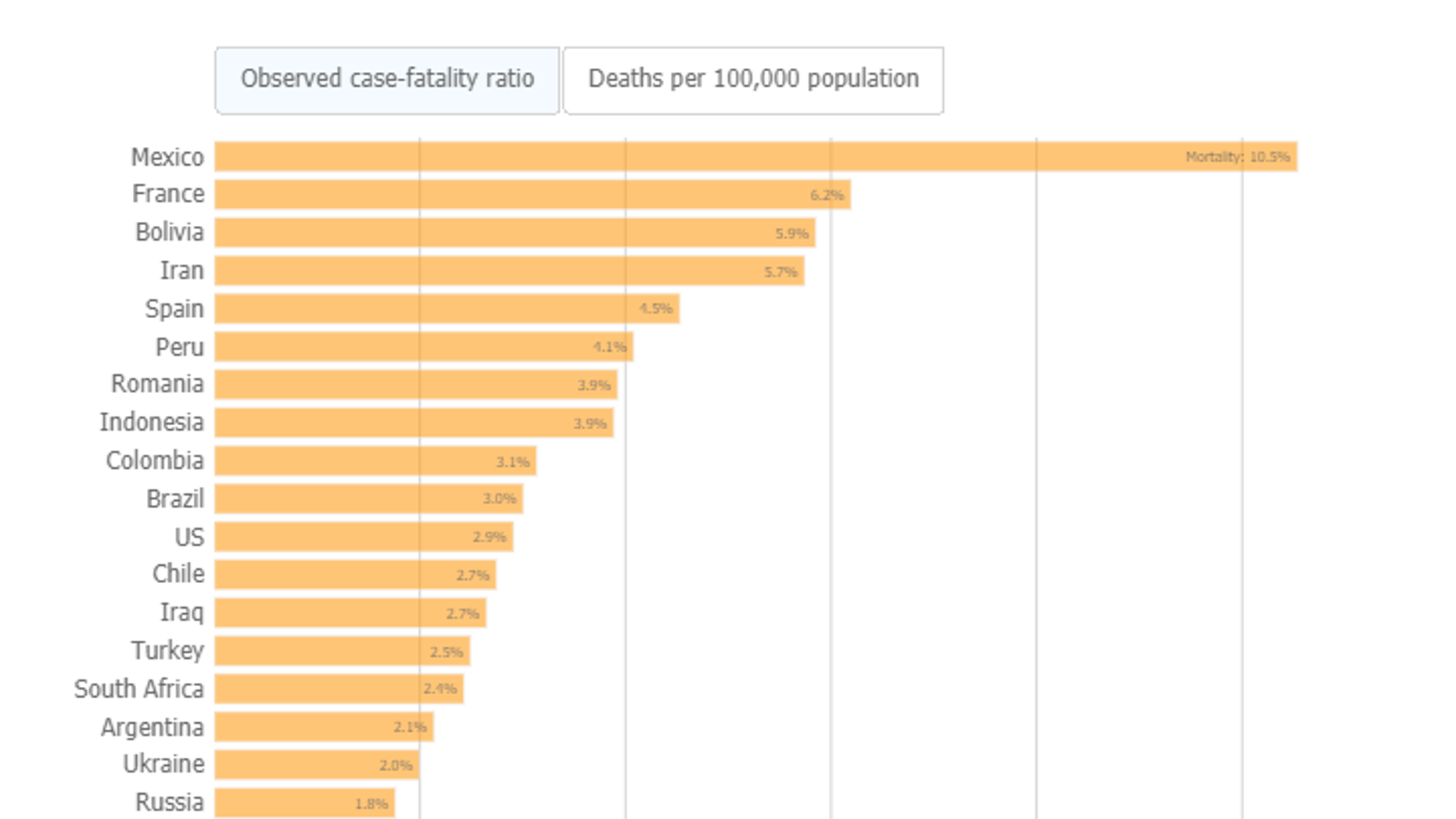
Source: US coronavirus case-fatality ratio ranks 11th in Johns Hopkins mortality analysis
_________________
Author of Practical Preparations for a Coronavirus Pandemic.
A very unique plan. As Dr. Paul Thompson wrote, "This is the very best paper on the virus I have ever seen."
COVID Mortality in U.S. by Geological Region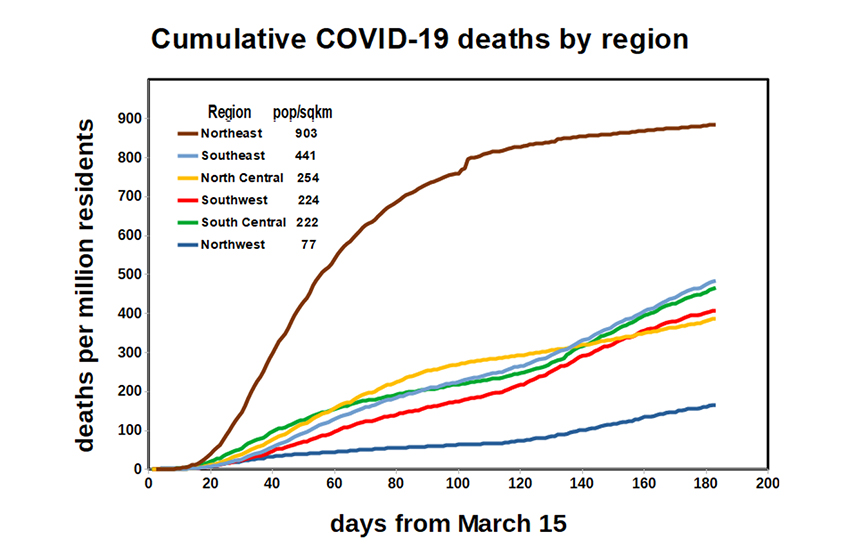
The Northeast suffered from being first and overwhelmed – those early deaths remain reflected in the cumulative totals. Masking and social distancing kicked in by early summer. Midsummer saw premature lifting and widespread flouting of exposure restrictions in the South – as those three widely separated southern regions show a rise in deaths at about Day 120.
Trends are roughly parallel in the three northern regions, but cumulative deaths doubled from Northwest to North Central and again to Northeast. The Northeast is the most crowded region of the country, the northwest the least. The estimated urban population densities (listed on the graph) increase about 5-fold in each case.
The message is clear; COVID-19's mortality is related to our crowding and behavior. Not all of us can change our geography. What to do if you live in a high population density? Wear your mask and avoid crowds.
Source: Every Picture Tells A Story: For COVID-19 Mortality, Does Geography Matter?
From my perspective, there are two important variables at work here. First, the deadliest regions in the U.S. is the Northeast which is most reliant on mass transit. So once the infection took root, it spread there like wildfire. The second variable was timing. It struck the Northeast in the winter when humidity levels were low. But when it began to spread to other regions and they began to deal with the virus, the mortality rate was depressed because the nation had moved into the spring and summer months.
_________________
Author of Practical Preparations for a Coronavirus Pandemic.
A very unique plan. As Dr. Paul Thompson wrote, "This is the very best paper on the virus I have ever seen."
Asymptomatic Carriers
I came across an interesting article yesterday but I was too busy helping my wife remodel the kitchen to talk about it.
One of the problems with trying to stop the infectious spread of the Coronavirus is individuals that do not show symptoms. They are called asymptomatic carriers. According to one study: [Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Yokohama, Japan, 2020], the percentage of asymptomatic carriers was 17.9%. That is very high. It means that you have to treat everyone as if they were infected.
The article that I read yesterday, expands on this asymptomatic population.
The analysis, published in PLOS Medicine and conducted by researchers with the University of Bern in Switzerland, suggests that some patients described as asymptomatic at the time of the study period may later go on to develop symptoms but are unaccounted for in the data. In other words, they are not asymptomatic but rather pre-symptomatic. As many as four in five will go on to develop symptoms. Source: Most coronavirus patients will develop symptoms, study analysis argues
_________________
Author of Practical Preparations for a Coronavirus Pandemic.
A very unique plan. As Dr. Paul Thompson wrote, "This is the very best paper on the virus I have ever seen."
ASPartOfMe
Veteran

Joined: 25 Aug 2013
Age: 66
Gender: Male
Posts: 34,465
Location: Long Island, New York
U.S. hits 7,000,000 COVID-19 cases
The seven-day average of new coronavirus cases dipped below 40,000-per-day for the first time since June on Sept. 11, the day America marked the 19th anniversary of the Al Qaeda terror attacks. By Friday it was back over 40,000 again. There were 43,670 new cases reported Wednesday.
Florida reopens state's economy despite ongoing pandemic
DeSantis, a major ally of President Donald Trump, acknowledged that the pandemic is far from over, but he said the threat has eased and the time has come to reopen for business after six months of “people twisting in the wind.”
Florida's governor expects 'full Super Bowl' in Tampa next year
New York Threatens Orthodox Jewish Areas With Lockdown Over Virus
Mayor Bill de Blasio ordered the Police Department and the Sheriff’s Office to enforce public health guidelines in several Orthodox Jewish neighborhoods in Queens and Brooklyn, where residents often do not wear masks or engage in social distancing. But community leaders said residents have been resisting the guidelines because of hostility toward Mr. de Blasio and the growing influence of President Trump, whose views on masks and the pandemic have been widely embraced.
Officials this week released statistics showing that the positivity rate in some Orthodox Jewish neighborhoods had grown to anywhere from 3 percent to 6 percent, significantly more than the city’s overall rate of between 1 percent and 2 percent.
Mr. de Blasio said on Friday on The Brian Lehrer Show that the city had closed four yeshivas over violations of social distancing rules.
Visits to Borough Park showed how the rules are often ignored. The coronavirus outbreak devastated New York’s Orthodox Jewish community in March and April, and community leaders say hundreds have died, including influential religious leaders. But this week, there was hardly a face mask in sight, as if the pandemic had never happened.
Borough Park and Midwood were islands of support for President Trump during the 2016 election, when the president won 89 percent of the vote in one local precinct.
_________________
Professionally Identified and joined WP August 26, 2013
DSM 5: Autism Spectrum Disorder, DSM IV: Aspergers Moderate Severity
It is Autism Acceptance Month
“My autism is not a superpower. It also isn’t some kind of god-forsaken, endless fountain of suffering inflicted on my family. It’s just part of who I am as a person”. - Sara Luterman
In my state, Indiana, the governor has announced that the state is moving to Phase 5 (the final stage) of the reopening plan. The implementation took place today September 26. The face mask order will still be in place.
Indiana State Medical Association president Dr. Roberto Darroca said in an emailed statement that the state positivity rate for cases has declined to less than 4%. It was at 6.4% when Holcomb first issued the mask mandate.
The positivity rate provides a window into how pervasive the virus is in a community, measuring the total number of tests divided by the number of people who test positivity. Higher positivity rates suggest greater virus circulation and or too little testing. The World Health Organization has said that governments not reopen until the positivity rate is lower than 5% for at least two weeks.
Given the current positivity rate, Darroca said, the medical association supports Holcomb's decision to move ahead with the state's Back on Track plan.
Source: What public health experts say about Indiana's move to Stage 5: 'Not out of the woods'
So essentially our state is returning back to normal or at least as normal as possible during the pandemic.
I went and saw my 6th film at the movie theater since the lockdown began to be lifted. It was a little more crowded then at the beginning. There were two other movie goers in the audience. It was just me and my N95 being free to live my life as close to normal as I can.
My daughter finally had the REME-HALO air purifier system installed into her HVAC system at her home. It will go a long ways towards making her home coronavirus proof for the second wave when we transition into the winter months.
_________________
Author of Practical Preparations for a Coronavirus Pandemic.
A very unique plan. As Dr. Paul Thompson wrote, "This is the very best paper on the virus I have ever seen."





