Emergence of a Deadly Coronavirus
Blood Type
One study in China examined 206 people in Wuhan who died from the virus and there were 63% more Blood type A fatal cases than Blood type O. People with Type A blood are more susceptible to a particular kind of lung disease, which happens to be triggered by the novel coronavirus that causes COVID-19.
There are four different ABO blood types: A, B, AB, and O. These types depend on the sort of glycoproteins (that is, proteins covered with sugars) that decorate red blood cells (RBCs). A person with Type A blood has only the "A" glycoprotein, a person with Type B blood has only the "B" glycoprotein, a person with Type AB has both, and a person with Type O has neither. Blood type is genetically determined by your mother and father.
It has long been known that susceptibility to infectious disease varies by blood type. Specifically, critically ill Type A patients are likelier to develop acute respiratory distress syndrome (ARDS), in which the lungs fill with fluid and are unable to adequately supply the blood with oxygen. ARDS is also often the cause of death in patients with COVID-19. One reason is related to the number of A glycoproteins on the surface of red blood cells and other body cells. There are subtypes of Type A blood. One gene (A1) results in much more of the A glycoprotein on cell surfaces than the other gene (A2). The scientists found that the higher the density of these A glycoproteins, the likelier it is that a sick patient will develop ARDS.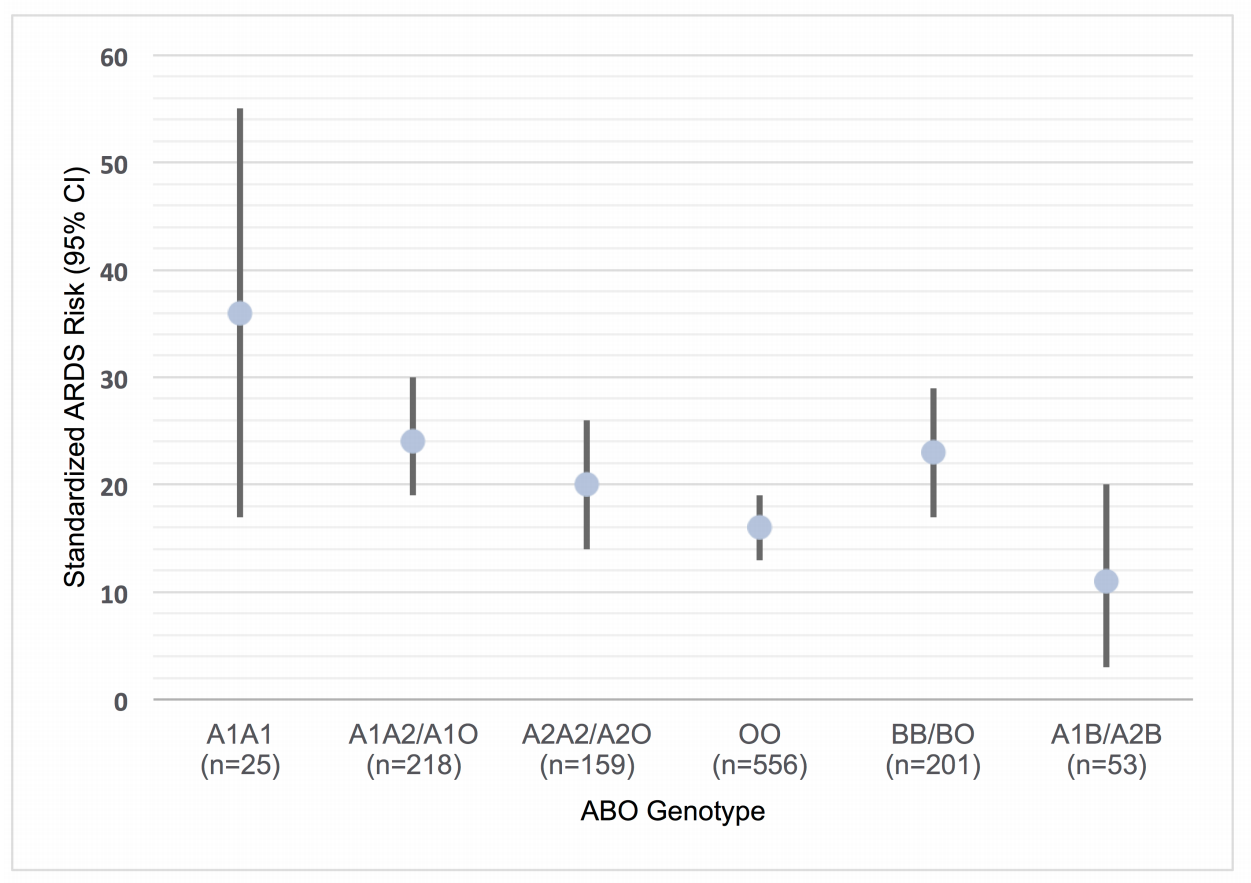
Sources:
* Does blood type matter when it comes to coronavirus? A Chinese study says yes
* Blood Type A Is Linked To Severe Lung Disease, Like That Caused By COVID
_________________
Author of Practical Preparations for a Coronavirus Pandemic.
A very unique plan. As Dr. Paul Thompson wrote, "This is the very best paper on the virus I have ever seen."
Moderna Vaccine
Moderna said its vaccine appears to be 94.5% effective, according to preliminary data from the company's still ongoing study. A week ago, competitor Pfizer Inc. announced its own COVID-19 vaccine appeared similarly effective — news that puts both companies on track to seek permission within weeks for emergency use in the U.S.
Source: Live Updates: Moderna coronavirus vaccine is 94.5% effective, company reports
_________________
Author of Practical Preparations for a Coronavirus Pandemic.
A very unique plan. As Dr. Paul Thompson wrote, "This is the very best paper on the virus I have ever seen."
The Atlantic published an interesting article:
Pfizer and BioNTech have announced a stunning success rate in their early Phase 3 vaccine trials—if it holds up, it will be a game changer. Treatments have gotten better too. A monoclonal antibody drug—similar to what President Donald Trump and former Governor Chris Christie received—just earned emergency-use authorization from the FDA. Dexamethasone—a cheap, generic corticosteroid—cut the death rate by a third for severe COVID-19 cases in a clinical trial.
Doctors and nurses have much more expertise in managing cases, even in using nonmedical interventions like proning, which can improve patients’ breathing capacity simply by positioning them facedown. Health-care workers are also practicing fortified infection-control protocols, including universal masking in medical settings.
Our testing capacity has greatly expanded, and people are getting their results much more quickly. We may soon get cheaper, saliva-based rapid tests that people can administer on their own, itself a potential game changer.
It might also be time for ordinary people to consider using higher-quality masks (N95s and KN95s)—something that public-health experts have long recommended. [since when?*] This is especially true for low-wage workers, a disproportionate number of whom are people of color and have to work indoors; older people, and anyone who works with them; and people with preexisting conditions that put them at higher risk.
Source: It’s Time to Hunker Down
* The World Health Organization (WHO) initially advised that the average person does not need to wear face mask. They later changed their guidance to everyone should wear cloth face mask (the wrong type of mask). As far as I know they haven't changed their guidance to the right type of mask, the N95. CDC follows after WHO. N95s can protect you from the virus and that is the type the so called experts should have recommended from day 1.
_________________
Author of Practical Preparations for a Coronavirus Pandemic.
A very unique plan. As Dr. Paul Thompson wrote, "This is the very best paper on the virus I have ever seen."
Infections at WHO Headquarters
The World Health Organization has recorded 65 cases of the coronavirus among staff based at its headquarters, including at least one cluster of infections, an internal email obtained by The Associated Press shows, despite the agency's past assertions that there has been no transmission at the Geneva site.
The email did not specify who was infected, but a WHO staffer with direct knowledge of the situation who spoke on condition of anonymity because she was not authorized to speak to the press said the cluster included a member of the WHO director-general’s leadership team who is also an infection control specialist.
Source: Email: 65 virus cases, with 1 cluster, in WHO Geneva staff
_________________
Author of Practical Preparations for a Coronavirus Pandemic.
A very unique plan. As Dr. Paul Thompson wrote, "This is the very best paper on the virus I have ever seen."
ASPartOfMe
Veteran

Joined: 25 Aug 2013
Age: 66
Gender: Male
Posts: 34,480
Location: Long Island, New York
Emergency rooms are starting to fill again with COVID-19 patients. Utah, where Nathan Hatton is a pulmonary specialist at the University of Utah Hospital, is currently reporting 2,500 confirmed cases a day, roughly four times its summer peak.
Hospitals have put their pandemic plans into action, adding more beds and creating makeshift COVID-19 wards. But in the hardest-hit areas, there are simply not enough doctors, nurses, and other specialists to staff those beds. Some health-care workers told me that COVID-19 patients are the sickest people they’ve ever cared for: They require twice as much attention as a typical intensive-care-unit patient, for three times the normal length of stay. “It was doable over the summer, but now it’s just too much,” says Whitney Neville, a nurse based in Iowa.
The entire state of Iowa is now out of staffed beds, Eli Perencevich, an infectious-disease doctor at the University of Iowa, told me. Worse is coming. . With only lax policies in place, those cases will continue to rise. Hospitalizations lag behind cases by about two weeks; by Thanksgiving, today’s soaring cases will be overwhelming hospitals that already cannot cope. “The wave hasn’t even crashed down on us yet,” Perencevich said. “It keeps rising and rising, and we’re all running on fear. The health-care system in Iowa is going to collapse, no question.”
Smaller clinics, nursing homes, and long-term-care facilities are still struggling to provide personal protective equipment, including gloves and masks. “About a third are completely out of at least one type of PPE” despite having COVID-19 cases, says Esther Choo, a physician at Oregon Health and Science University and a founder of Get Us PPE.
If death rates have fallen thanks to increasing medical savvy, they might rise again as nurses and doctors burn out. “If we can get patients into staffed beds, I feel like they’re doing better,” Perencevich said. “But that requires a functional health-care system, and we’re at the point where we aren’t going to have that.”
None of these drugs is for treating COVID-19 itself. “That’s just to keep them alive,” Neville, the Iowa nurse, said. An ICU nurse can typically care for two people at a time, but a single COVID-19 patient can consume their full attention. Those patients remain in the ICU for three times the length of the usual stay.
Nurses and doctors are also falling sick themselves. “The winter is traditionally a very stressful time in health care, and everyone gets taken down at some point,” says Saskia Popescu, an infection preventionist at George Mason University, who is based in Arizona. The third COVID-19 surge has intensified this seasonal cycle, as health-care workers catch the virus, often from outside the hospital. “Our unplanned time off is double what it was last October,” says Allison Suttle of Sanford Health, a health system operating in South Dakota, North Dakota, and Minnesota. Many hospitals have staff on triple backup: While off their shifts, they should expect to get called in if a colleague and their first substitute and the substitute’s substitute are all sick. At least 1,375 U.S. health-care workers have died from COVID-19.
The first two surges were concentrated in specific parts of the country, so beleaguered hospitals could call for help from states that weren’t besieged. People were coming to us in our hour of need,” says Madad, from NYC Health + Hospitals, “but now the entire nation is on fire.” No one has reinforcements to send.
Making matters worse, patients with other medical problems are sicker than usual, several doctors told me. During the earlier surges, hospitals canceled elective surgeries and pulled in doctors from outpatient clinics. People with heart problems, cancers, strokes, and other diseases found it harder to get medical help, and some sat on their illness for fear of contracting COVID-19 at the hospital. Now health-care workers are facing an influx of unusually sick people at a time when COVID-19 has consumed their attention and their facilities.
For many health-care workers, the toll of the pandemic goes beyond physical exhaustion. COVID-19 has eaten away at the emotional core of their work. “To be a nurse, you really have to care about people,” Neville said. But when an ICU is packed with COVID-19 patients, most of whom are likely to die, “to protect yourself, you just shut down. You get to the point when you realize that you’ve become a machine. There’s only so many bags you can zip.”
Even after cases stop climbing, health-care workers will have to catch up on a new round of procedures that didn’t happen because of COVID-19—but without the adrenaline that a packed hospital brings. “Everyone talks about fatigue during the surge, but one of the hardest things is coming down from it,” Popescu says. “You’re exhausted but you still don’t get that mental break.”
As hard as the work fatigue is, the “societal fatigue” is harder, said Hatton, the Utah pulmonary specialist. He is tired of walking out of an ICU where COVID-19 has killed another patient, and walking into a grocery store where he hears people saying it doesn’t exist. Health-care workers and public-health officials have received threats and abusive messages accusing them of fearmongering. They’ve watched as friends have adopted Donald Trump’s lies about doctors juking the hospitalization numbers to get more money. They’ve pleaded with family members to wear masks and physically distance, lest they end up competing for ICU beds that no longer exist. “Nurses have been the most trusted profession for 18 years in a row, which is now BS because no one is listening to us,” Neville said.
Bolding=mine
_________________
Professionally Identified and joined WP August 26, 2013
DSM 5: Autism Spectrum Disorder, DSM IV: Aspergers Moderate Severity
It is Autism Acceptance Month
“My autism is not a superpower. It also isn’t some kind of god-forsaken, endless fountain of suffering inflicted on my family. It’s just part of who I am as a person”. - Sara Luterman
In my region, most people follow the rules. They wear masks and obey social distancing. And yet the coronavirus infection rate is exploding. So perhaps one might hit the PAUSE button and ponder if the rules really do prevent the virus transmission.
From my perspective, they do not. The virus is an airborne virus and is spread by aerosols. Until the so called medical experts acknowledge this fact and redesign their guidance, the infections will expand as we enter the winter months.
Does wearing a face mask stop the virus. NO, not unless it is the right kind of face mask such as an N95.
Ventilating indoor spaces is important.
Maintaining indoor humidity levels above 40% RH in the winter is important.
Social distancing is important.
Sanitizing indoor air using UVC light is important.
Focusing efforts on the most vulnerable instead of locking down the entire population is important.
Streamlining rapid treatment for the most vulnerable is important.
_________________
Author of Practical Preparations for a Coronavirus Pandemic.
A very unique plan. As Dr. Paul Thompson wrote, "This is the very best paper on the virus I have ever seen."
The Second Wave
Coronavirus infections are exploding in the U.S. as we approach the Winter.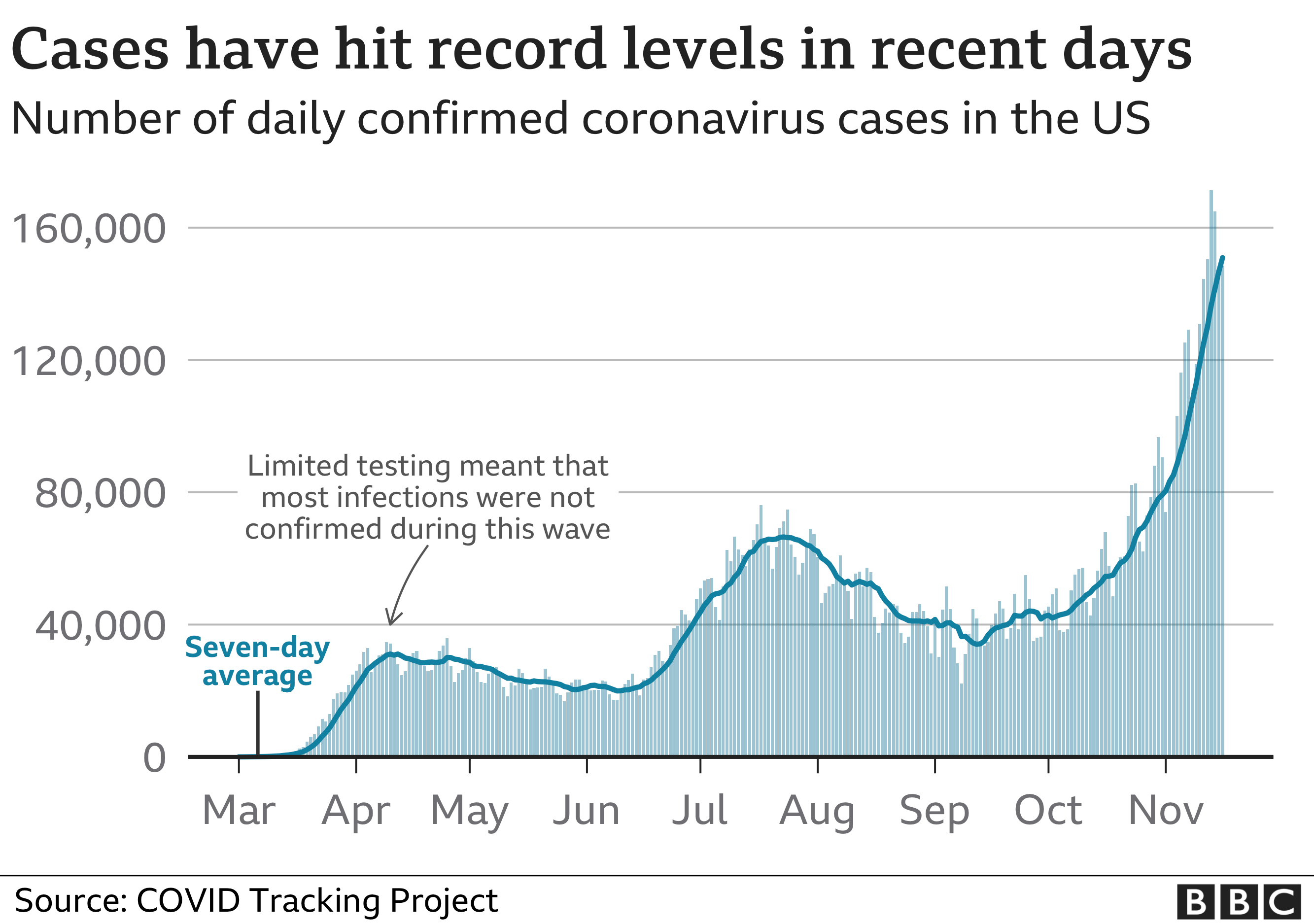
During the spring wave, testing was mostly limited to confirming cases in people who were already in hospital, meaning the true scale of that outbreak wasn't fully captured.
But the latest data compiled by the COVID Tracking Project shows the current surge is not just down to increased testing - the number of tests carried out in the US was up by 12.5% week on week, while the number of cases increased by more than 40%.
One likely cause is the change of season and colder weather driving people indoors to socialise, where the risk of spread is heightened due to less social distancing and poor ventilation.
Source: Covid-19 in the US: Is this coronavirus wave the worst yet?
_________________
Author of Practical Preparations for a Coronavirus Pandemic.
A very unique plan. As Dr. Paul Thompson wrote, "This is the very best paper on the virus I have ever seen."
Pfizer's Vaccine Delivery Pilot Program
Pfizer's vaccine, which was shown to be more than 90% effective in preventing COVID-19 based on initial data, must be shipped and stored at -70 degrees Celsius (minus 94°F), significantly below the standard for vaccines of 2-8 degrees Celsius (36-46°F). This represents some significant challenges. As a result the company is implementing a pilot program to assess the logistical problems of distribution.
Pfizer Inc has launched a pilot delivery program for its experimental COVID-19 vaccine in four U.S. states, as the U.S. drugmaker seeks to address distribution challenges facing its ultra-cold storage requirements.
It picked Rhode Island, Texas, New Mexico, and Tennessee for the program after taking into account their differences in overall size, diversity of populations, immunization infrastructure, and need to reach individuals in varied urban and rural settings. The company expects to have enough safety data on the vaccine from the ongoing large scale late-stage trials by the third week of November before proceeding to apply for emergency use authorization (EUA).
Source: Pfizer to start pilot delivery program for its COVID-19 vaccine in four states
Former FDA commissioner and Pfizer board member Scott Gottlieb suggested the entry of two "highly effective" vaccines into the market—namely Pfizer's and Moderna's—"could effectively end this pandemic in 2021," CNBC reports. Gottlieb's prediction hinges on the efficacy of those mRNA-based shots once full data are released, combined with the fact that many people will have already had COVID-19 by 2021.
Source: Pharma COVID-19 tracker: Pfizer tees off vaccine delivery pilot; CureVac plots European shot manufacturing network
_________________
Author of Practical Preparations for a Coronavirus Pandemic.
A very unique plan. As Dr. Paul Thompson wrote, "This is the very best paper on the virus I have ever seen."
ASPartOfMe
Veteran

Joined: 25 Aug 2013
Age: 66
Gender: Male
Posts: 34,480
Location: Long Island, New York
Mouthwash 'can kill virus in lab in 30 seconds'
Scientists at Cardiff University found there were "promising signs" that over-the-counter mouthwashes may help to destroy the virus.
The report comes ahead of a clinical trial on Covid-19 on patients at the University Hospital of Wales.
Dr Nick Claydon said the study could lead to mouthwash becoming an important part of people's routines.
While the research suggests use of mouthwash may help kill the virus in saliva, there is not evidence it could be used as a treatment for coronavirus, as it will not reach the the respiratory tract or the lungs.
The university report states that mouthwashes containing at least 0.07% cetypyridinium chloride (CPC) showed "promising signs" of being able to eradicate the virus when exposed to the virus in a lab.
While the report is yet to be peer reviewed, it supports another recent study which found CPC-based mouthwashes are effective in reducing viral load.
Dr Richard Stanton, lead author on the study, said: "This study adds to the emerging literature that several commonly-available mouthwashes designed to fight gum disease can also inactivate the SARS-CoV-2 coronavirus (and other related coronaviruses) when tested in the laboratory under conditions that are designed to mimic the oral/nasal cavity in a test tube.
The NYC Schools are doing it right
amny
_________________
Professionally Identified and joined WP August 26, 2013
DSM 5: Autism Spectrum Disorder, DSM IV: Aspergers Moderate Severity
It is Autism Acceptance Month
“My autism is not a superpower. It also isn’t some kind of god-forsaken, endless fountain of suffering inflicted on my family. It’s just part of who I am as a person”. - Sara Luterman
Another example of a Superspreader event due to Aerosols
At least 32 people who attended a wedding in Ohio last month have reportedly contracted the coronavirus, including the bride and groom and two of the couple’s grandparents who had to visit the emergency room for severe symptoms. A third grandparent also tested positive for the virus but didn't have to go to the hospital. Anthony and Mikayla Bishop cut their wedding party guest list down from 200 to 85 before they were married on Oct. 31 in Blue Ash, a city in the suburbs of Cincinnati.
She said they offered masks to their guests but hardly anyone wore them. When her parents walked her down the aisle she said she looked at the guests’ faces and realized, “Nobody's wearing a mask. I'm walking down the aisle. We can't do anything now." Despite the fact that their grandparents were the only ones wearing masks the whole time, they still got sick, Mikayla Bishop said. "They actually wore their mask except for when they were eating their dinner."
Source: Ohio wedding linked to at least 32 coronavirus cases: 'Nobody's wearing a mask'
In a crowded venue, viral particles in aerosol form will float in the air for hours like cigarette smoke. People will breathe in the viral particles deep inside their throat and lungs and become infected. Wearing masks is not effective unless one is wearing the right kind of mask such as an N95. Otherwise the event transforms into a superspreader event.
_________________
Author of Practical Preparations for a Coronavirus Pandemic.
A very unique plan. As Dr. Paul Thompson wrote, "This is the very best paper on the virus I have ever seen."
Enduring Immunity
In a study published to the pre-preprint server bioRxiv on Monday, researchers said that immunity against SARS-CoV-2, the virus that causes a COVID-19 infection, could last for at least six months, or it could be longer, perhaps a matter of years. Researchers analyzed various aspects of immunity, including antibodies, B cells and two types of T cells. T cells respond to a foreign invader such as a virus but are different from antibodies and are thought to provide immunity against the coronavirus for a longer period of time. By the end, the researchers noted that antibodies were “durable,” showing only modest declines after six to eight months. The antibody responses among the participants “spanned a 200-fold range,” the researchers said in the study.
The findings are “also consistent with the recent detection of SARS-CoV T cells 17 years after the initial infection.” In other words, the findings are in line with a recent discovery that survivors of the SARS outbreak in the early 2000s still had T cells against that coronavirus more than a decade after recovering.
Source: Coronavirus immunity could last more than 6 months, possibly years: study
_________________
Author of Practical Preparations for a Coronavirus Pandemic.
A very unique plan. As Dr. Paul Thompson wrote, "This is the very best paper on the virus I have ever seen."
250,000 people have died in the USA as of today.
Actually closer to 2,500,000. Considering about 7,500 people die each day in the USA.
Aerosol Transmission
In a nutshell, SARS-CoV-2 will be more able to survive and spread this winter due to lower temperatures, combined with reduced humidity and drier conditions inside your breathing passages (respiratory tract). As the weather gets colder, the air gets drier and retains less humidity. When we turn on the heat in our homes, it further dries the air and the cells and tissues inside our nose, airway passages, reducing the ability of one of our natural defenses—mucus—from removing viruses such as SARS-CoV-2 as well as other debris and viruses, and bacteria.
Research on influenza and MERS indicates that there is a higher chance of developing infections when the relative humidity declines from about 40-60% (typical in warmer weather) to about 20%. Case reports from China and Seattle during the early days of the pandemic also noted similar findings. A cohort climate modeling study published in JAMA looking at 50 international cities also confirmed that SARS-CoV-2 is more stable and remains on certain receptors in our airways as the relative humidity drops and stays at 20%. This also explains why we are more apt to contract cold viruses and influenza in colder temperatures.
The minimum lower limit of indoor relative humidity (RH) in public buildings should be 40-60%, an important way to reduce the transmission of respiratory infections. At 0-40% relative humidity, airborne droplets containing viruses shrink by evaporation, become lighter and stay afloat for longer periods of time, increasing the risk of infection and transmission. But at 40-60% relative humidity, these airborne droplets containing viruses are much heavier and fall out of the air to the ground, reducing the potential for transmission.
Source: Dry Air Indoors Will Increase Transmission Of Covid-19 As Winter Approaches
_________________
Author of Practical Preparations for a Coronavirus Pandemic.
A very unique plan. As Dr. Paul Thompson wrote, "This is the very best paper on the virus I have ever seen."
The Dose Makes the Poison
How many viruses we are initially infected with is a key determinant of how sick we get, according to evidence from other viruses and animal studies. We also know this is true in hamsters that have been experimentally infected with SARS-CoV-2.
Imagine if you touch a door handle that happens to have one virus particle on it and then touch your nose and breathe that particle in. You will be infected with that one virus particle. One estimate, published in the Lancet, suggested one SARS-CoV-2 virus particle will have replicated to make nearly 30 new virus particles in 24 hours. Those 30 new particles can then go on to infect 30 more cells, giving rise to 900 new particles in the next 24 hours or so.
Now imagine someone sneezes right in your face and you inhale 1,000 virus particles. After one round of replication you could have 30,000 particles, and then 900,000 in the round after. In the same period of time, your body could be dealing with 1,000 times more compared to the first scenario.
Once the immune system detects the virus, it has to race to get it under control and stop it replicating. It does this in three main ways:
* telling our cells how to disrupt viral replication
* making antibodies that recognize and neutralize the virus to stop it infecting more cells
* making T cells that specifically kill virus-infected cells.
While the first step is relatively quick, creating specific antibodies and T cells take days or even weeks. Meanwhile, the virus is replicating over and over again. So the initial dose of the virus really determines how much of the body the virus has infected before the immune system kicks fully into gear.
People infected with SARS-CoV-2, the virus that causes Covid-19, can spread the virus when they speak, sing, cough, sneeze, or even just breathe. Scientists think face masks help the limit virus spread by protecting everyone else from the infected wearer. As a result, face masks are now mandatory in many cities, states, and countries to limit the spread of Covid-19.
People typically wear surgical, cloth, or other face coverings that don’t completely prevent the virus from infecting the wearer, though medical grade surgical masks do appear to offer more protection. Nonetheless, these don’t have the same level of protection as N95 or P2 “respirator” masks worn by many healthcare workers. Additionally, how we wear the mask matters, as touching it often and not completely covering the nose and mouth renders it ineffective.
While these face coverings may not completely prevent us from getting infected with Covid-19, they probably reduce the number of virus particles we inhale — the “viral dose.” Scientists think a lower viral dose can reduce the severity of the disease we get. Indeed, where universal face masking is implemented, a much higher proportion of new infections with Covid-19 are asymptomatic.
Source: How wearing a mask could build immunity to Covid-19
_________________
Author of Practical Preparations for a Coronavirus Pandemic.
A very unique plan. As Dr. Paul Thompson wrote, "This is the very best paper on the virus I have ever seen."






